Please feel free to add the profile of anyone living with or who lived with Rheumatoid Arthritis
What is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is an autoimmune disease in which the body’s immune system – which normally protects its health by attacking foreign substances like bacteria and viruses – mistakenly attacks the joints. This creates inflammation that causes the tissue that lines the inside of joints (the synovium) to thicken, resulting in swelling and pain in and around the joints. The synovium makes a fluid that lubricates joints and helps them move smoothly.
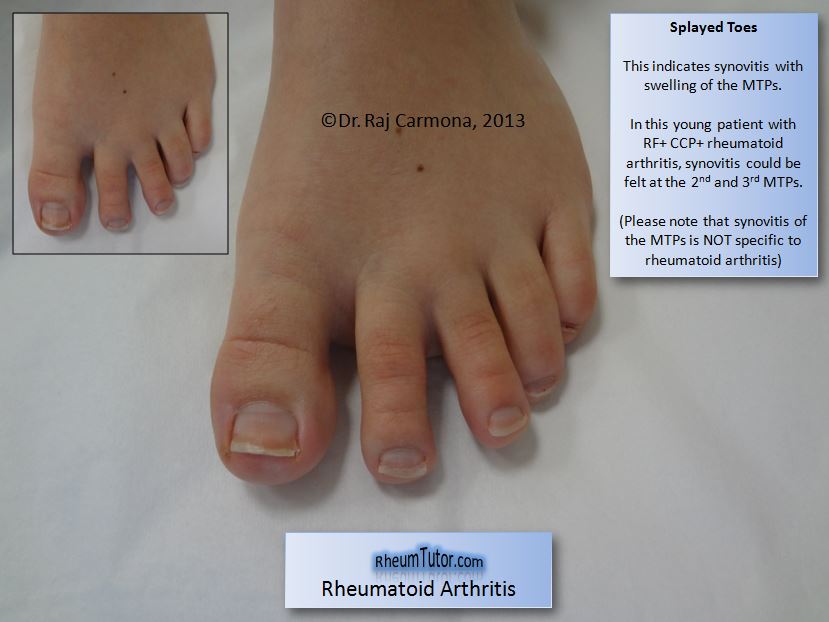
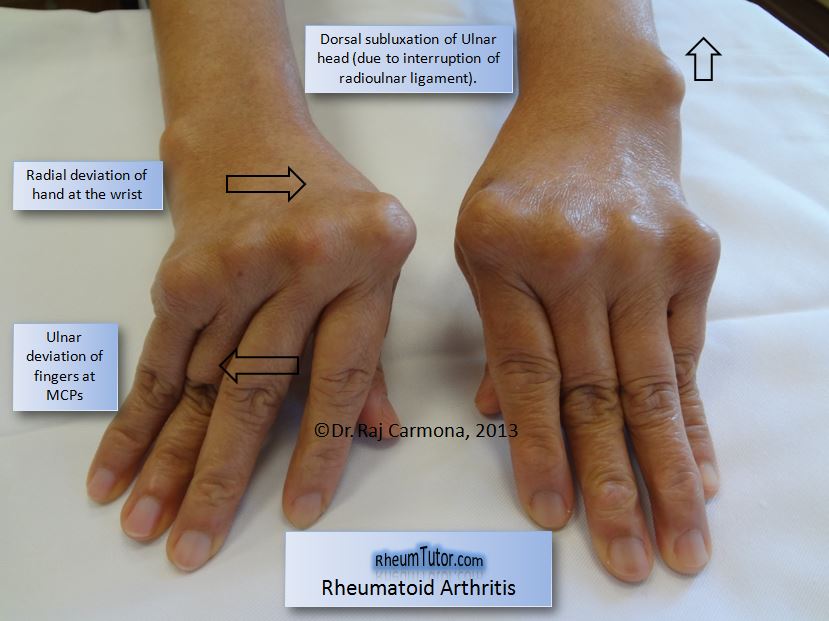
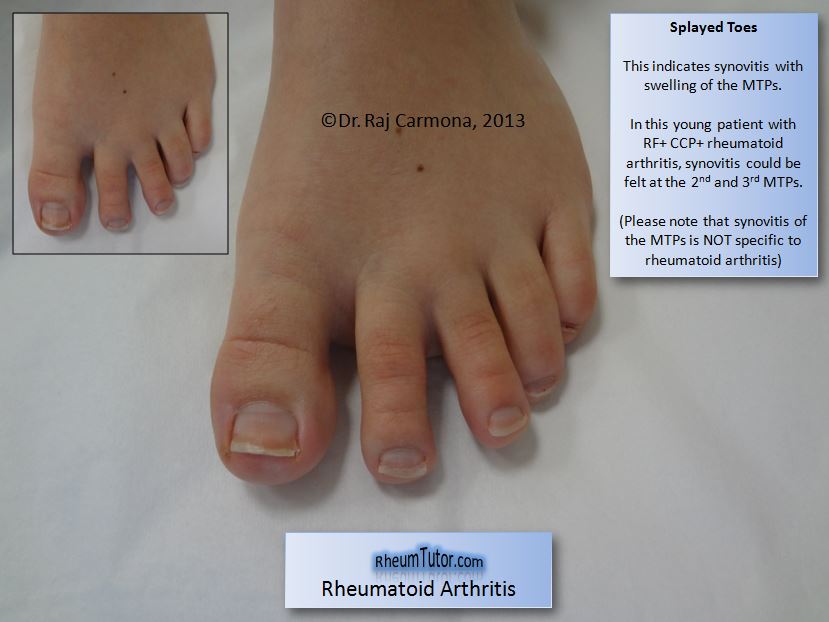
Rheumatoid arthritis most commonly affects the joints of the hands, feet, wrists, elbows, knees and ankles. The joint effect is usually symmetrical. That means if one knee or hand if affected, usually the other one is, too. Because RA also can affect body systems, such as the cardiovascular or respiratory systems, it is called a systemic disease. Systemic means “entire body.”
Who’s Affected by Rheumatoid Arthritis?
About 1.5 million people in the United States have rheumatoid arthritis (RA). Nearly three times as many women have the disease as men. In women, RA most commonly begins between ages 30 and 60. In men, it often occurs later in life. Having a family member with RA increases the odds of having RA. However, most people with RA have no family history of the disease.
Rheumatoid Arthritis Symptoms
The early stages, people with RA may not initially see redness or swelling in the joints, but they may experience tenderness and pain.
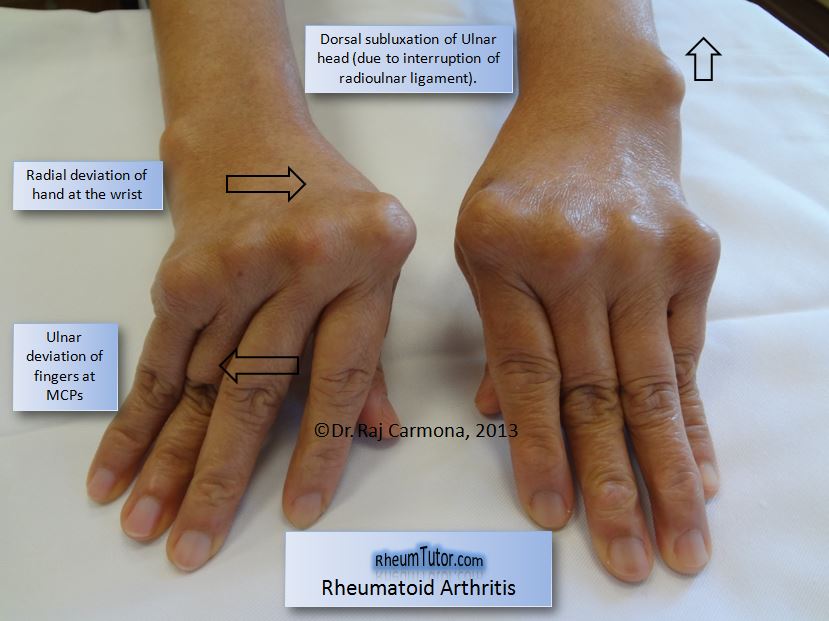
These following joint symptoms are clues to RA: Joint pain, tenderness, swelling or stiffness for six weeks or longer
Morning stiffness for 30 minutes or longer
More than one joint is affected
Small joints (wrists, certain joints of the hands and feet) are affected
The same joints on both sides of the body are affected
Along with pain, many people experience fatigue, loss of appetite and a low-grade fever. The symptoms and effects of RA may come and go. A period of high disease activity (increases in inflammation and other symptoms) is called a flare. A flare can last for days or months.
Systemic problems caused by Rheumatoid Arthritis
Bone Thinning – Chronic inflammation from RA leads to loss of bone density, not only around the joints, but throughout the body, leading to thin, brittle bones. Exercise, a high-calcium diet and vitamin D can all help bones, but in some cases your doctor may need to prescribe a drug to stimulate bone growth or prevent bone loss.
Eyes –
- Inflammation and scarring. Some people with RA develop inflammation of the whites of the eyes (scleritis) that can lead to scarring.
- Symptoms include:
- Pain
- Redness
- Blurred vision
- Light sensitivity
- Scleritis is usually treatable with medications prescribed by your doctor, but in rare cases, the eye may be permanently damaged.
- RA can also cause uveitis - an inflammation of the area between the retina and the white of the eye, which, if not treated, could cause blindness.
- Dryness. The inflammatory process that affects the joints can also damage the tear-producing glands, a condition known as Sjögren’s syndrome. The result is eyes that feel dry and gritty. Artificial tears as well as oral medications available, over the counter or by prescription can relieve symptoms.
Mouth –
- Inflammation can damage the moisture-producing glands of the mouth resulting in a dry mouth, tooth decay, gum disease, and halitosis. Over-the-counter artificial saliva products and self-treatment often helps. If not, your doctor may prescribe a medication to increase the production of saliva.
Skin –
- Nodules - About half of people with RA develop rheumatoid nodules – lumps of tissue that form under the skin, often over bony areas, but sometimes they form in the lungs and are usually harmless.
- Rashes - When RA-related inflammation of the blood vessels (called vasculitis) affects the skin, a rash of small red dots is the result. In more severe cases, vasculitis can cause skin ulcers on the legs or under the nails.
Lungs –
- Inflammation and scarring: Up to 80 percent of people with RA have some degree of lung involvement, which is usually not severe enough to cause symptom. However, prolonged inflammation can lead to a form of lung disease called pulmonary fibrosis that interferes with breathing and can be difficult to treat.
Heart and Blood Vessels –
- Atherosclerosis - Chronic inflammation can damage endothelial cells that line the blood vessels, causing the vessels to absorb more cholesterol and form plaques.
- Heart attack and stroke. When plaques from damaged blood vessels break loose they can block a vessel leading to heart attack or stroke.
- In fact, a 2010 Swedish study found that the risk of heart attack for people with RA was 60 percent higher just one year after being diagnosed with RA.
- Pericarditis. Inflammation of the heart lining, the pericardium, may manifest as chest pain. Treatment to control arthritis often controls pericarditis as well.
- Anemia - Unchecked inflammation can lead to a reduction in red blood cells characterized by headache and fatigue.
- Treatment consists of drugs to control inflammation along with iron supplements.
- Blood clots - Inflammation might lead to elevated blood platelet levels, and blood clots. Felty syndrome – is usually described as associated with or a complication of rheumatoid arthritis. This disorder is generally defined by the presence of three conditions:
- Rheumatoid arthritis (RA)
- An enlarged spleen (splenomegaly)
- Low white blood cell count. Treatment consists of Immunosuppressant drugs.
Nervous System - Pinched or compressed nerves.
- Although RA does not directly affect the nerves, inflammation of tissues may cause compression of the nerves resulting in numbness or tingling, such as carpal tunnel syndrome.
Drug effects – RA medications, including cyclosporine, methotrexate, other DMARDS, biologics, NSAIDS, corticosteroids, and acetaminophen may reduce inflammation and pain in people with RA. However, they all have their risk as shown below.
Liver failure –
- The long-term use of acetaminophen.
- Long-term methotrexate use.
Kidneys disease –
- Cyclosporine
- Methotrexate
- NSAIDs
Corticosteroids effects -
- Thinning of the skin
- Susceptibility to bruising
- Sun sensitivity
- A rash at the injection site
Mortality - RA reduces lifespan on average from three to twelve years.4 According to the UK's National Rheumatoid Arthritis Society, Young age at onset, long disease duration, the concurrent presence of other health problems (called co-morbidity), and characteristics of severe RA—such as poor functional ability or overall health status, a lot of joint damage on x-rays, the need for hospitalization, or involvement of organs other than the joints—have been shown to associate with higher mortality. Positive responses to treatment may indicate a better prognosis. A 2005 study by the Mayo Clinic noted that RA sufferers suffer a doubled risk of heart disease, independent of other risk factors such as diabetes, alcohol abuse, and elevated cholesterol, blood pressure and body mass index. The mechanism by which RA causes this increased risk remains unknown; the presence of chronic inflammation has been proposed as a contributing factor.[5] It is possible that the use of new biologic drug therapies extend the lifespan of people with RA and reduce the risk and progression of atherosclerosis. This is based on cohort and registry studies, and still remains hypothetical.
Rheumatoid Arthritis Causes
The cause of RA is not yet fully understood, although doctors do know that an abnormal response of the immune system plays a leading role in the inflammation and joint damage that occurs. No one knows for sure why the immune system goes awry, but there is scientific evidence that genes, hormones and environmental factors are involved.
Researchers have shown that people with a specific genetic marker called the HLA shared epitope have a fivefold greater chance of developing rheumatoid arthritis than do people without the marker. The HLA genetic site controls immune responses. Other genes connected to RA include: STAT4, a gene that plays important roles in the regulation and activation of the immune system; TRAF1 and C5, two genes relevant to chronic inflammation; and PTPN22, a gene associated with both the development and progression of rheumatoid arthritis. Yet not all people with these genes develop RA and not all people with the condition have these genes.
Researchers continue to investigate other factors that may play a role. These factors include infectious agents such as bacteria or viruses, which may trigger development of the disease in a person whose genes make them more likely to get it; female hormones (70 percent of people with RA are women); obesity; and the body’s response to stressful events such as physical or emotional trauma. Research also has indicated that environmental factors may play a role in one's risk for rheumatoid arthritis. Some include exposure to cigarette smoke, air pollution, insecticides and occupational exposures to mineral oil and silica.
 Researchers at University of California San Diego School of Medicine (May 2018) and the Icahn School of Medicine at Mount Sinai, using analytic tools, have decoded the epigenetic landscape for rheumatoid arthritis (RA). In unveiling RA's epigenome—the proteins and molecules that decorate DNA and help turn genes on and off—scientists made a surprising discovery: an overlap between the causes of RA and Huntington's disease, a fatal and incurable genetic brain disease.
Researchers at University of California San Diego School of Medicine (May 2018) and the Icahn School of Medicine at Mount Sinai, using analytic tools, have decoded the epigenetic landscape for rheumatoid arthritis (RA). In unveiling RA's epigenome—the proteins and molecules that decorate DNA and help turn genes on and off—scientists made a surprising discovery: an overlap between the causes of RA and Huntington's disease, a fatal and incurable genetic brain disease.
"By revealing the comprehensive epigenetics behind rheumatoid arthritis, we now have a better understanding of this disease. More importantly, our new approach, could not only help patients with rheumatoid arthritis, but also people with other immune-mediated diseases," Firestein said.
History
The first known traces of arthritis date back at least as far as 4500 BC. A text dated 123 AD first describes symptoms very similar to RA.
It was noted in skeletal remains of Native Americans found in Tennessee. In Europe, the disease is vanishingly rare before the 17th century.
The first recognized description of RA in modern medicine was in 1800 by the French physician Dr Augustin Jacob Landré-Beauvais(1772–1840) who was based in the famed Salpêtrière Hospital in Paris. The name "rheumatoid arthritis" itself was coined in 1859 by British rheumatologist Dr Alfred Baring Garrod.
An anomaly has been noticed from the investigation of Pre-Columbian bones. The bones from the Tennessee site show no signs of tuberculosis even though it was prevalent at the time throughout the Americas.
Historic treatments for RA have included; rest, ice, compression, elevation, apple diet, nutmeg, some light exercise every now and then, nettles, bee venom, copper bracelets, rhubarb diet, extractions of teeth, fasting, honey, vitamins, insulin, magnets, and electroconvulsive therapy, ETC.
Etymology
Rheumatoid arthritis is derived from the Greek word ῥεύμα-rheuma (nom.), ῥεύματος-rheumatos (gen.) ("flow, current"). The suffix -oid ("resembling") gives the translation as joint inflammation that resembles rheumatic fever. Rhuma which means watery discharge might refer to the fact that the joints are swollen or that the disease may be made worse by wet weather.
Notables
- Lucille Désirée MORTON (Ball) - (1911-1989), a legend in the comedy world, who was known for her physical comedy and energy playing Lucy on" I Love Lucy," also struggled with rheumatoid arthritis since the age of 17
- Camryn Manheim - best known for her role as Ellenor Frutt on the law drama TV show “The Practice,” spoke out about her struggle with rheumatoid arthritis in 2005 in People magazine. Diagnosed at 44, Camryn experienced stiffness, pain and fatigue, all tell-tale signs of rheumatoid arthritis, but wasn’t diagnosed for eight months.
- Mary Kathleen TURNER - a famous actress who was at the height of her career in the 1980s, with films such as “Romancing the Stone,” “Body Heat” and “Peggy Sue Got Married,” was diagnosed with RA in the 1990s. In 2002 she spearheaded an RA awareness campaign to educate about the disease.
- James Coburn - (1928-2002) was a famous actor particularly in the 1960s, where he appeared in many action and western movies, such as “The Magnificent Seven” and “The Great Escape.” In the arthritis world, Coburn was known for making grand statements about curing his rheumatoid arthritis with alternative treatments.
- Rosalind Russell - (1907-1976) was a famous stage and movie actress, who rose to fame in the 1930s. Her most notable performances were in the movies “His Girl Friday” and “Auntie Mame.” She was also nominated for five Golden Globes and won all of them. She was diagnosed with rheumatoid arthritis in 1969, and died of breast cancer with complications from her RA in 1976.
- Aida Turturro - Best known for her role as Tony Soprano’s sister Janice on the HBO show, “The Sopranos,” Turturro teamed up with the Arthritis Foundation as a national spokesperson for rheumatoid arthritis in 2000. Turturro was diagnosed with RA when she was 12
- Pier-Auguste Renoir - (1841-1919), the famous 19th century French artist is known for his impressionist paintings. Though his first bout with rheumatoid arthritis struck around 1898, he continued to paint and create artwork his entire life. His RA was severe and crippling, but he found creative ways to paint despite his pain and deformed hands.
- Kristy McPherson - is a professional golfer who was diagnosed with systemic-onset juvenile arthritis at age 11. She is currently playing on the LPGA Tour. She has said she took up golf because after being diagnosed, she was no longer able to play sports that involved running and jumping.
- Meredith Boyd - Crowned Mrs. Georgia International in 2008, Boyd is now a beauty queen and a spokesperson for the Arthritis Foundation. Diagnosed as a teen, Boyd has had surgery to ease her pain, but cannot take RA meds due to another condition.
- Glenn Frey - known as a founding member of the popular rock band the Eagles. He died in 2016 due to complications of his RA, ulcerative colitis, and pneumonia.
References & Additional Reading:
- Arthritis.org - How RA affects the body
- WebMD - What is Felty Syndrome
- MedicalExpress News - A link between Huntington's disease and rheumatoid arthritis
- Amy M. Wasserman (2011). Diagnosis and Management of Rheumatoid Arthritis.
- Cardiac disease in rheumatoid arthritis. Johns Hopkins University. 2002. Archived from the original on October 9, 2006
- Rothschild, Bruce M. Tennessee Origins of Rheumatoid Arthritis Mcclungmuseum.utk.edu. Archived from the original on February 2, 2012. Retrieved March 3, 2011.
- [https://web.archive.org/web/20030219095659/http:/www.arc.org.uk/new..."Bones of contention"] Arthritis Research UK. April 1999. Archived from the original on February 19, 2003. Retrieved February 5, 2013.
- Garrod AB (1859). The Nature and Treatment of Gout and Rheumatic Gout. London: Walton and Maberly.
- Rothschild BM, Rothschild C, Helbling M; Rothschild; Helbling (2003). "Unified theory of the origins of erosive arthritis: conditioning as a protective/directing mechanism?”. J. Rheumatol 30 (10): 2095–102. PMID 14528501.
- Wikipedia - The art of Peter Paul Rubens
- Hart FD (1976). "History of the treatment of rheumatoid arthritis.. Br Med J. 1 (6012): 763–5.
- History the treatment of Rheumatoid Arthritis. PMC 1639217. PMID]
- Paget, Stephen A.; Lockshin, Michael D.; Loebl, Suzanne (2002). The Hospital for Special Surgery Rheumatoid Arthritis Handbook Everything You Need to Know. New York: John Wiley & Sons. p. 32. ISBN 9780471223344. Archived from the original on 2017-02-22.
- Healthline - Those with Rheumatoid Arthritis More Likely to Die Early
- Healthline - Arthritis - What’s rheumatoid arthritis?
- Wikipedia - Rheumatoid arthritis







 Researchers at University of California San Diego School of Medicine (May 2018) and the Icahn School of Medicine at Mount Sinai, using analytic tools, have decoded the epigenetic landscape for rheumatoid arthritis (RA). In unveiling RA's epigenome—the proteins and molecules that decorate DNA and help turn genes on and off—scientists made a surprising discovery: an overlap between the causes of RA and Huntington's disease, a fatal and incurable genetic brain disease.
Researchers at University of California San Diego School of Medicine (May 2018) and the Icahn School of Medicine at Mount Sinai, using analytic tools, have decoded the epigenetic landscape for rheumatoid arthritis (RA). In unveiling RA's epigenome—the proteins and molecules that decorate DNA and help turn genes on and off—scientists made a surprising discovery: an overlap between the causes of RA and Huntington's disease, a fatal and incurable genetic brain disease.